Building a culture of clinician well-being: strategies, technology, and leadership that work

Ed Lee
Chief Medical Officer

Kenza Bouzoubaa
Brand & Communication Manager
On March 19, 2025, Nabla & HealthLeaders hosted a discussion in recognition of Health Workforce Well-Being Day, bringing together leading voices in healthcare to explore strategies and tools for improving clinician well-being. The webinar, titled Health Workforce Well-Being Day 2025: Strategies and Tools for Health System Leaders to Build a Culture of Clinician Well-Being, featured expert panelists who shared their insights on the pressing issue of burnout in healthcare and the role of technology in addressing it.
The growing urgency of clinician well-being
Moderated by Eric Wicklund, Senior Innovation and Technology Editor at Health Leaders, the conversation brought together:
- Dr. Ed Lee, MD, MPH, Chief Medical Officer at Nabla
- Dr. John Chuck, MD, Chief Wellness Officer & Professor of Family Medicine at California Northstate University College of Medicine
- Dr. Hugo Gomez, MD, MSc, PhD, Board-certified Adult Psychiatrist at Harbor Psychiatry and Mental Health
- Dr. Matthew Sakumoto, MD, Virtualist & CMIO at Sutter West Bay Region
The panelists agreed that clinician burnout has long been an issue, but the COVID-19 pandemic accelerated the crisis. Increased administrative burdens, growing documentation requirements, and emotional fatigue have made it clear that healthcare must prioritize workforce well-being beyond just a single day of recognition.
Beyond the "pizza party" approach
The panelists stressed that health systems must go beyond superficial wellness initiatives—like pizza parties or mindfulness workshops—and address structural issues such as workload management, administrative burden, and institutional culture.
Dr. Chuck emphasized the importance of leadership commitment:
Well-being needs to be a top-down priority. It’s not just about making clinicians more ‘resilient’—it’s about redesigning systems to support them.
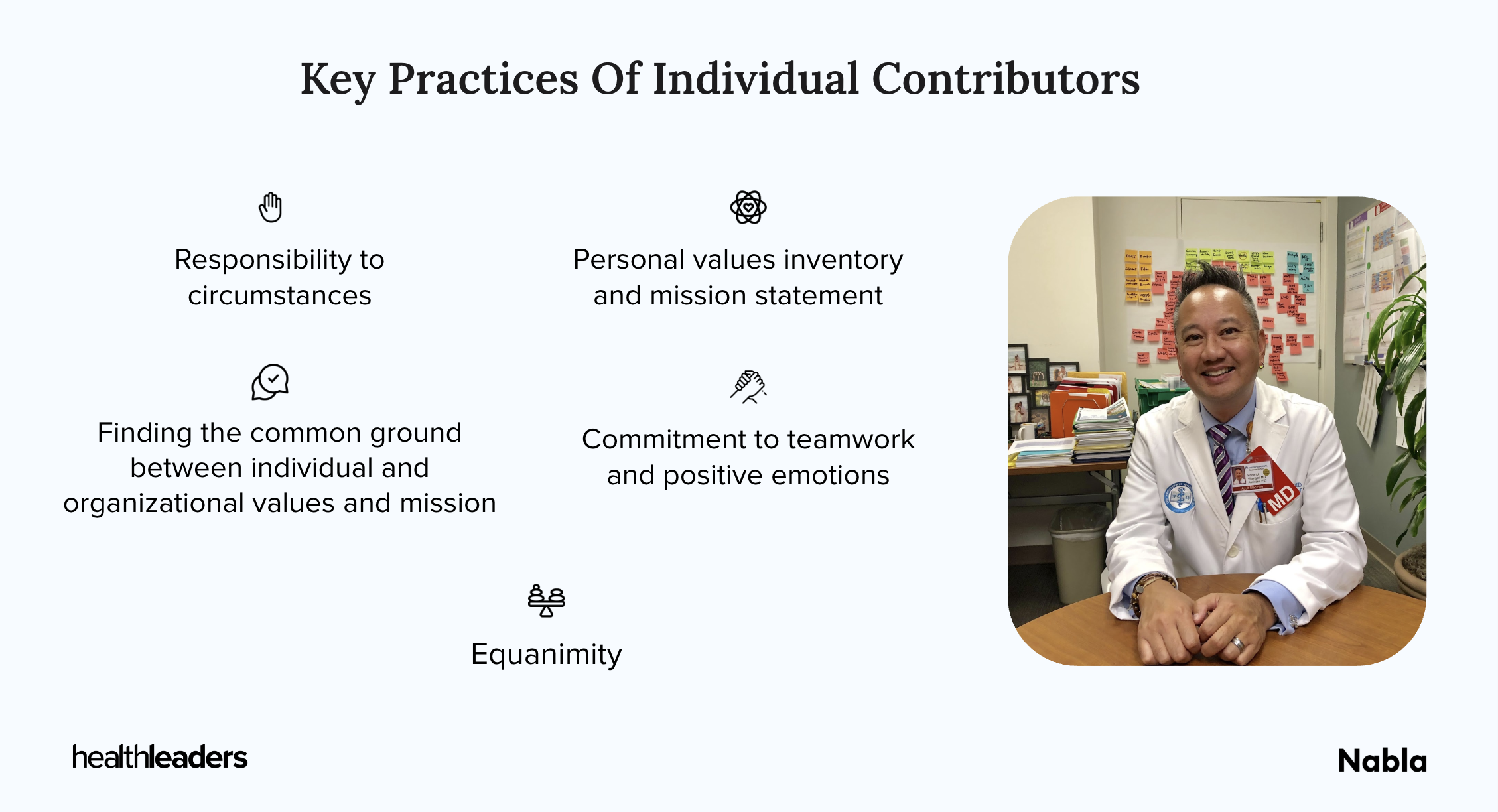
He also reminded us that wellness isn’t just the job of one person:
Every individual in an organization, from top to bottom, side to side, needs to play a role in wellness and to see themselves as a wellness leader.
He added:
This is how we change cultures and operations: it starts with words and conversations, which shape operations and culture.
Ambient AI: a game changer for clinician workflows
A key focus of the discussion was how ambient AI technology is helping alleviate administrative burdens.
Dr. Lee highlighted the impact Nabla has already had:
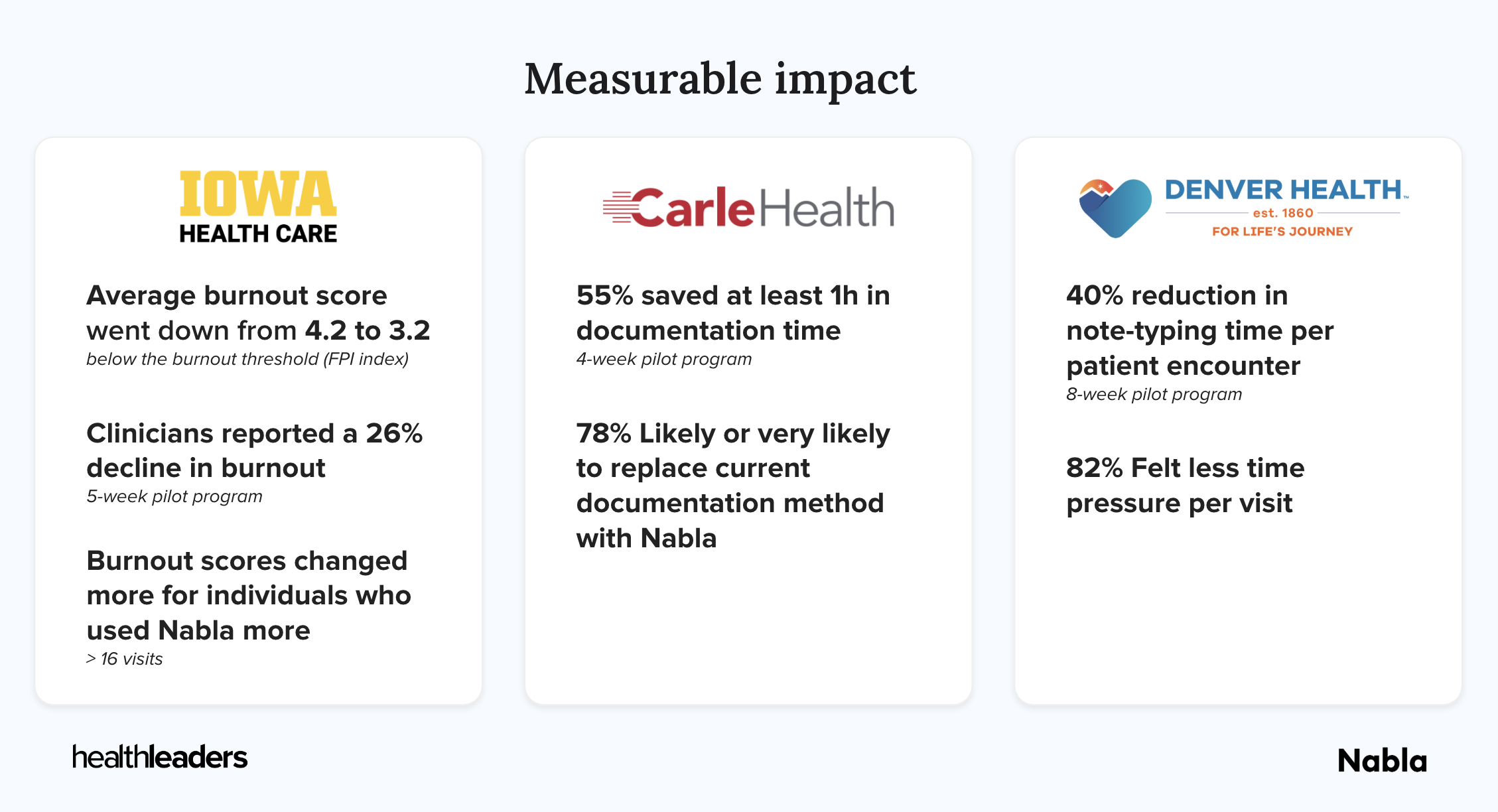
Clinicians using Nabla have reported significant reductions in documentation time, allowing them to spend more time with patients and less time on paperwork. It’s about giving them their evenings back.
Health systems that have implemented Nabla have seen notable decreases in burnout. Dr. Lee shared the example of The University of Iowa Health Care which reported a 26% reduction in burnout after just five weeks of use.
The key to AI adoption, according to Dr. Sakumoto, is seamless integration into existing workflows:
We need technology that doesn’t add to the cognitive burden but instead reduces it.
Dr. Gomez echoed this, saying:
I feel like a practitioner again. I can practice medicine—not just document. That’s the most powerful feedback I’ve received.
Creating a sustainable culture of well-being
Dr. Gomez shared his perspective as a psychiatrist, noting that eye contact and human connection are often sacrificed when clinicians are buried in documentation. AI solutions like Nabla allow providers to fully engage with their patients without worrying about missing details in their notes.
Dr. Chuck emphasized that wellness isn’t only a moral obligation—it’s a sound financial strategy. He cited research showing that burnout-driven physician turnover costs health systems between $500,000 and $1 million per provider (AMA).
Dr. Lee expanded on the downstream effects:
Burned-out clinicians are less effective, less efficient, and more prone to absenteeism and medical errors. This impacts patient satisfaction, loyalty, and ultimately, revenue. The overall financial impact of clinician burnout extends beyond individual organizations.
The path forward: actionable strategies
To conclude the discussion, panelists outlined actionable strategies for organizations looking to prioritize clinician well-being:
- Empower leadership to make well-being a strategic priority with measurable goals.
- Promote shared ownership of well-being across the organization, where every team member—not just leadership—is a champion for wellness.
- Use EHR data to identify at-risk clinicians who are suffering in silence.
- Invest in AI-powered documentation solutions to reduce administrative burden.
- Move beyond token wellness initiatives and invest in systemic changes that make daily work more manageable.
Dr. Chuck also reflected on the immeasurable value of immersive retreats:
People arrive dejected and leave smiling. That’s not something you measure with a bathroom scale—you measure it through stories, culture, and the hope it restores.
Dr. Sakumoto highlighted:
The best tech solutions don’t require two-hour training or major workflow changes. It should take 15 minutes to get up and running and start seeing impact.
Final thoughts
The consensus among panelists was clear: the future of healthcare depends on taking clinician well-being seriously. AI is emerging as a powerful tool in this fight, but its success hinges on thoughtful implementation and a commitment from healthcare leaders to truly transform the way clinicians work.
Dr. Chuck shared a message he often tells his medical students:
Your future is going to be much better than my past.
He reflected on how tools like ambient AI are helping to reshape the clinical experience, giving the next generation of providers more time for meaningful patient interactions and less time buried in documentation.
Dr. Lee summed it up best:
Well-being should not be a once-a-year event. It should be embedded in the culture of every healthcare organization.
For those who missed the webinar, here is the full recording: